 |
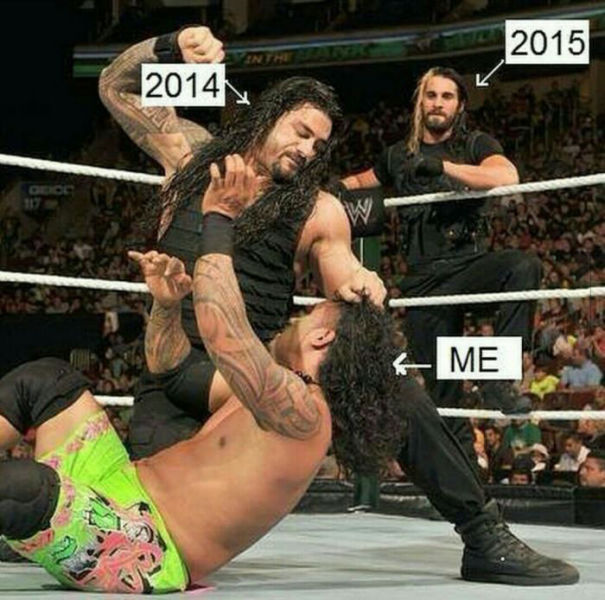
| Me vs Pulmonary Hypertension |
When I started this blog another person with Pulmonary Hypertension told me to keep it light- no one wants to hear you complain or cry. While this advice is sound- it is difficult to explain how this process has been without sounding like I am complaining. Truthfully- the past year has sucked. There is no way around it. There is not a nice way to word it. It sucked- and that is okay. Things are allowed to suck. You are allowed to have a bad year- and it is okay to own it. So, if you don't want to hear about my year (which most people would categorize as the physical shits) I would skip this post and continue with your day.
Being diagnosed with Pulmonary Hypertension, especially so suddenly and at such a severe stage proves complex and difficult. It has complicated all of my relationships, and sometimes I carry a lot of guilt. I know this disease isn't just hard on me. It is hard on my parents, my family, my boyfriend, and the few remaining friends I have left.
Someone who cares deeply about me deeply told me the other day that sometimes he thinks that I am faking. I was initially hurt by his words, but then I thought about it. Other than the oxygen, I look completely the same. He has no idea how I feel, and even if I were to describe how I physically feel, he will not truly understand how it feels because he is not in my position. He will not understand that even though I look fine, I am exhausted from working harder than him just to breathe all day. Something like a wheelchair is a visual cue to others that someone is not able to use their legs. When you have a heart/lung disease there is no visual cue.
In the movie Maleficent, the main character has wings because she is a fairy. One day someone she trusted cuts off her wings in her sleep. When she wakes up and discovers her wings are gone she lets out a giant scream and sobs while holding her back where her wings once were. It sounds silly, but I really related to this scene. It felts as if someone, somewhere, decided someday to take away my ability to use my heart and lungs properly. When you are unable to breathe properly- it is hard to do many physical things that you one enjoyed. I can't explain to you how much I miss my independence and exploring the world around me.What hurts more is not being able to do a basic task, like dress myself without supplementary oxygen. Doing so without oxygen leaves me breathless and my lips blue. It is a shitty feeling for anyone. It is something you never expect to happen to you, especially at such a young age. My sense of normalcy has been taken from me, and I don't know why. Sometimes I wonder if I did something wrong to do deserve this. Was it something I ate? Was it karma? Was my name drawn from a hat?
I am in a long-term relationship with a wonderful young man who is in his 20s. He has been as supportive as he knows how, and I am thankful for that. I know it takes a lot of love and faith to stay with someone with a condition with mine- and I know that not even marriage makes people stay in situations like this. I obviously have some guilt about someone so young choosing to stay with me. I don't know what my health will be like in the future. I cannot give him biological children. I really don't know what could happen. I don't know what kind of future I could give to him, or promise him- or anyone.
 Not many people have the life experience of dating someone with a serious chronic life-threatening disease. Oddly enough, this is something that I do have experience with. I was in a relationship with someone for nearly 6 years who had childhood cancer. There were a few scares that his cancer returned, this seemed to happen around Christmas (just like my diagnosis.) One year, the year I was supposed to apply to university, the scare seemed more serious than the others. They had to run more tests- and we were obviously very scared and worried. This is a story I have never told anyone else... I shared with a woman at work about the potential cancer scare with my boyfriend at the time, and she shared with me that she too had dated someone with cancer. She said that he was the love of her life- but she couldn't stay with him. She felt it was too much of a gamble to love someone who was more likely to get sick- and perhaps, die. She advised me to do the same and said I should break up with him before things get worse. In a weird way, her advice helped me because I disagreed with it so strongly. Her advice taught me to love everyone as much as I can in all the time that we have together- which is a beautiful lesson that not everyone is brave enough to follow. This woman chose not to spend the rest of her life, with the love her life out of fear. After that I chose to do whatever I could to help. I decided not to apply to university just in case the next round of results were not what we were hoping for. I was prepared to put my life on hold and take care of him, because everything else would be waiting at the end if he did need treatment. Luckily, his cancer did not return. I went to university a year later...I had an early acceptance and was offered multiple scholarships. Everything was waiting for me a year later.
Not many people have the life experience of dating someone with a serious chronic life-threatening disease. Oddly enough, this is something that I do have experience with. I was in a relationship with someone for nearly 6 years who had childhood cancer. There were a few scares that his cancer returned, this seemed to happen around Christmas (just like my diagnosis.) One year, the year I was supposed to apply to university, the scare seemed more serious than the others. They had to run more tests- and we were obviously very scared and worried. This is a story I have never told anyone else... I shared with a woman at work about the potential cancer scare with my boyfriend at the time, and she shared with me that she too had dated someone with cancer. She said that he was the love of her life- but she couldn't stay with him. She felt it was too much of a gamble to love someone who was more likely to get sick- and perhaps, die. She advised me to do the same and said I should break up with him before things get worse. In a weird way, her advice helped me because I disagreed with it so strongly. Her advice taught me to love everyone as much as I can in all the time that we have together- which is a beautiful lesson that not everyone is brave enough to follow. This woman chose not to spend the rest of her life, with the love her life out of fear. After that I chose to do whatever I could to help. I decided not to apply to university just in case the next round of results were not what we were hoping for. I was prepared to put my life on hold and take care of him, because everything else would be waiting at the end if he did need treatment. Luckily, his cancer did not return. I went to university a year later...I had an early acceptance and was offered multiple scholarships. Everything was waiting for me a year later.As previously mentioned, I cannot carry children. Pregnancy increases the risk of mortality in women with PH. Earlier this year I was sent to a gynecologist office to discuss my birth control options. I was sent on a few months after diagnosis. The nurse there asked me how I was dealing with the diagnosis. I responded that it was a "total bummer." She gave me a look and asked "total bummer?" It is probably the worst thing that has ever happened to me, and that extends to those in my immediate circle who love me. Do I want to share this with a stranger? Not really- and I assume on some level a nurse understands the degree of suckage adjusting to that kind of diagnosis is. Being there was a horrible experience. The waiting room wall was plastered with faces of babies the office helped deliver. It dawned on me- this is a place people go for something joyous. I cried in the waiting room facing the pictures of children knowing I was there to prevent having my own because it is too dangerous. I cried speaking to the doctor about my options. It was too soon. (This was the second only time I cried at the doctors.) I imagine it is devastating to find out that pregnancy is too risky for most women of child baring age. I should mention that I have Teaching Preparation Specialization on my degree and worked at various child care centres- I was someone who obviously liked working with children and looked forward to being a parent. There has always been a desire to adopt. I am just worried I won't be healthy, stable or here long enough to be the mother I dreamed of being. However, there have been stories on this blog from other PHers who have adopted and they are 30-40+ diagnosis. How silly would it be if I let opportunities pass me by because I was afraid? What if I reach my goal of living to 87 years old and decided not to pursue anything because I was afraid I may not be here? That would be a life wasted. I am trying to learn that I cannot let fear decide my fate, nor can I let this disease decide my fate for me.
I like to end things on a positive note. Although this year has really sucked (like really sucked,) I haven't accepted defeat. As I mentioned in an earlier post I started to do Wii Fit Yoga as soon as I was able to stand again after diagnosis. I would have to do this at 4 liters of oxygen per minute. Now I walk for 20-40 minutes on a the Wii Fit bored on 2-2.5 litres of oxygen per minute. I can also box using a punching bag and do exercises on a Total Body Gym on the same amount of supplementary oxygen. I never thought I would be on oxygen for an entire year (or more,) but I have clearly made great improvements. I can sit completely without oxygen for the entire day. I have returned to work part-time and only use my oxygen to exit and enter the building. I am starting to do small tasks without oxygen, and my doctor is confident I will get off of it completely once my heart heals as it is. I was in bad shape and I suppose it will take sometime for my body to adapt and heal. I am looking forward to 2015. I am okay with one year out of my life being the physical shits. I plan on having many more, so one year out of 87 isn't bad.
I have also learned that I really really really like having control. Feeling as if a disease has control over me is not an option for me. As such, I have found ways to give me power back against Pulmonary Hypertension. I have done research on the characteristics of Cancer survivors (because no research of this exists for PH.) Oddly enough, a lot of the characteristics of Cancer survivors overlap with the qualities I have found in the PHers who have contributed their story to this blog! I have been trying to embrace those characteristics and incorporating alternative and complementary health care into my life. I have seen a naturopath, Bowen therapist, a CHEK practitioner, hypnotherapist and a healer. It might sound a little crazy- but why not try anything and everything if it is not dangerous? I also regularly get back massages at the fanciest spa in town and I think the world would be a better if everyone could get one. I journal everyday. I do at least 20-40 minutes of cardio everyday. I have altered my diet to suit my new needs. I meditate, I do breathing exercises. I practice self love and do what makes me happy. I say no to things I don't want to do, and use a bathbomb from Lush every Sunday. I do research about Pulmonary Hypertension, medication, so on and so forth and I am my own advocate.
I am not sure what 2015 has in store for me, but I am hopeful that this will be the year I complete my "comeback."













.jpg)



